Cardiac Rehabilitation Dialysis

・Graduated from Akita University School of Medicine in 1986
・Completed initial residency training at Okinawa Chubu Hospital
・Completed advanced internal medicine residency at the National Cardiovascular Center, Japan
・1991: Joined Dokkyo Medical University Saitama Medical Center, Department of General and Cardiovascular Medicine
・1996: Studied abroad at the University of California, San Diego, under the mentorship of Prof. Anthony N. DeMaria (Department of Cardiology) and Prof. Geert W. Schmid-Schönbein (Department of Bioengineering)
・2007: Appointed Associate Professor, Department of Clinical Pharmacology, Graduate School of Medicine, University of the Ryukyus
・2010: Appointed Associate Professor, Department of Cardiovascular, Renal, and Neurological Medicine, Graduate School of Medicine, University of the Ryukyus
・2012: Appointed Professor, Department of Cardiovascular, Vascular, and Renal Medicine, Dokkyo Medical University Nikko Medical Center
・Board Certified Specialist in Internal Medicine, Japanese Society of Internal Medicine
・Board Certified Cardiologist, Japanese Circulation Society
・Board Certified Specialist in Dialysis Therapy, Japanese Society for Dialysis Therapy
・Certified Instructor and Physician, Japanese Association of Cardiac Rehabilitation
Dokkyo Medical University Nikko Medical Center, located in the western region of Tochigi Prefecture, plays a vital role in delivering comprehensive regional healthcare. As a hospital deeply rooted in this community, the center is committed not only to providing acute care but also to strengthening chronic care management, with a particular focus on cardiac rehabilitation. While rehabilitation traditionally centers on the restoration of lost physical functions, cardiac rehabilitation at our center encompasses a dual approach. Approximately half of our efforts are dedicated to recovering patients’ physical capabilities. Equally important, the other half involves secondary prevention — a structured educational program aimed at minimizing the risk of recurrent cardiac events. This comprehensive rehabilitation strategy is fundamental to our patient management philosophy and represents a critical pathway in improving long-term cardiovascular outcomes.
Dr. Yasu: It is well established through extensive data that exercise therapy offers significant benefits to patients with cardiovascular disease. However, approximately 10–15% of patients are unable to participate in conventional exercise-based rehabilitation programs.
For these individuals, we explored various alternative approaches, but since introducing B-SES, it has proven to be an efficient and valuable substitute for exercise therapy. It allows us to provide a safe and effective treatment option tailored to patients who cannot engage in physical activity.
Dr. Yasu: The primary indications for B-SES include patients with heart failure, chronic peripheral artery disease of the lower limbs, and ischemic heart diseases such as angina pectoris and myocardial infarction — essentially those for whom physical exercise is particularly challenging.
In addition to these cardiovascular conditions, we often use B-SES for patients with comorbid pulmonary diseases, as well as elderly patients with orthopedic issues, such as severe knee osteoarthritis that makes walking difficult. These populations greatly benefit from this modality as part of their rehabilitation regimen.
Dr. Yasu: Comparative studies on B-SES have shown that patients who undergo this therapy tend to experience improvements in exercise tolerance and muscle strength. From my clinical perspective, one of its key advantages is the relatively rapid enhancement of muscle strength, which shortens the preparatory phase before patients can begin walking exercises or resistance training. This makes the rehabilitation process more efficient overall. In practical terms, this means we can reduce the length of hospital stays, which benefits not only healthcare economics but also improves patient and family satisfaction. Additionally, B-SES serves as an effective motivational tool, encouraging patients to move on to active rehabilitation with greater confidence. For those eligible to receive B-SES, it represents a highly promising therapeutic option.
Dr. Yasu: As a cardiologist, I’ve observed that B-SES is particularly effective for patients who fall between specialties — for example, those requiring both orthopedic and cardiovascular management, or those managing both diabetes and heart disease. The ability to provide cross-disciplinary rehabilitation with B-SES opens new avenues for care and delivers tangible benefits to these complex patient populations.
Dr. Yasu: B-SES is currently reimbursed as part of our comprehensive cardiac rehabilitation program under the existing healthcare coverage framework.
Dr. Yasu: The majority of patients who have undergone B-SES report high levels of satisfaction. While a small percentage — around 10% — initially express discomfort or difficulty with the electrical stimulation, most of these individuals gradually adapt through repeated sessions with lower-intensity settings and ultimately achieve meaningful therapeutic benefits.
Dr. Yasu: One of the major future applications of B-SES lies in supporting so-called “exercise-limited” patients — individuals who, until now, would have been confined to bed rest due to their inability to engage in conventional physical rehabilitation. By introducing B-SES, we can facilitate earlier mobilization and enable these patients to be discharged or transferred to care facilities much sooner. In terms of integrated healthcare and long-term care collaboration, for patients who have shown excellent outcomes with B-SES during hospitalization, we hope to extend this modality into care facilities, where its continued use would provide ongoing benefits. Additionally, for patients returning home, incorporating B-SES into home-based rehabilitation programs — alongside conventional training — offers a promising new direction for community-based cardiac and musculoskeletal rehabilitation.

Photo: Rehabilitation Room
• Graduated from the Department of Physical Therapy, Saitama Medical Welfare College in 2004
• Completed Doctoral Program in the Department of Internal Disorders, Graduate School of Medicine, Tohoku University in 2014 (Ph.D. in Medicine)
• 2013: Appointed Chief, Department of Rehabilitation, Dokkyo Medical University Nikko Medical Center
• Certified Instructor of Cardiac Rehabilitation
• Certified Hypertension and Cardiovascular Disease Prevention Educator
• Certified Health Science Advisor
• Certified Diabetes Educator
• Certified Respiratory Therapist
• Licensed Care Manager
The first key point is the preventive aspect — helping patients who have experienced heart disease to avoid a recurrence. However, our goal extends beyond simply preventing another cardiac event. We aim to support patients in regaining their roles in daily life, enabling them to return to work, enjoy their hobbies, and live fulfilling, active lives.
The second point applies to rehabilitation in general, particularly in our aging society. Hospitalized patients, especially older adults, tend to experience rapid physical deconditioning. To address this, cardiac rehabilitation focuses on two main strategies:
1.Early intervention to prevent disuse syndrome during hospitalization.
2.Prompt rehabilitation for those who have already developed disuse syndrome, in order to accelerate their recovery.
Cardiac rehabilitation, therefore, is not just about improving exercise tolerance. It also plays a vital role in maintaining and restoring physical function, cognitive function, and overall quality of life. Additionally, it contributes to preventing conditions such as dementia and falls. This comprehensive, multidisciplinary approach is increasingly expected of us in the field of cardiac rehabilitation.
Tamura, PT, PhD: In the field of cardiac rehabilitation, it’s essential for patients to engage in regular aerobic exercise and to build lasting exercise habits as part of their daily lives. However, the reality is that some patients simply dislike exercise. Others may be willing but unable to exercise adequately due to issues like knee pain. I had been searching for a way to help these patients engage in physical activity through a passive method, one that could still provide the benefits of exercise without placing additional strain on their bodies.
・Postoperative acute phase
・NYHA Class III–IV heart failure
・Cases with malnutrition
・High-risk cases related to exercise
・Patients with decreased ADL after hospitalization (wheelchair users)
・Frail patients whose ADL are improving
・Due to impaired motor function, the patient is unable to perform sufficient exercise; an additive effect to exercise therapy is expected, and the cardiac risk is low.
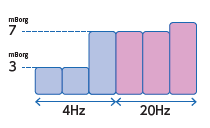
Tamura, PT, PhD: For patients in the acute phase following cardiac or vascular surgery, as well as those with severe heart failure classified as NYHA class III or IV, we avoid applying high-intensity loads. Specifically, we use the modified Borg scale (mBorg) to monitor patient discomfort and set exercise intensity accordingly. We maintain a very low intensity around mBorg 3—just enough to induce mild muscle contractions without causing discomfort—and apply this metabolic mode continuously.
By doing so, we aim to improve cachexia, the wasting syndrome often seen in chronic heart failure, which is associated with underlying inflammation. We expect B-SES to have anti-inflammatory effects. Rather than focusing on building muscle mass, the primary goal here is to prevent muscle catabolism—the breakdown of muscle tissue.
As rehabilitation progresses, for patients who still struggle with adequate nutrition or those who have improved their activities of daily living (ADL) but remain in a frail condition, we increase the intensity within this metabolic mode. Even then, the focus is more on improving muscle quality and enhancing neuromuscular function or nerve-muscle conduction, rather than simply increasing muscle size.
On the other hand, for patients with conditions such as osteoarthritis of the knee, who cannot walk sufficiently but have no significant cardiac issues, we switch from metabolic mode to disuse mode with the aim of increasing muscle strength and muscle mass. Typically, after patients have undergone metabolic mode three times, we transition to disuse mode. From there, we gradually increase the intensity, targeting a maximum of mBorg 7 or above.
Tamura, PT, PhD: Through the use of B-SES, I have observed that it synergistically On the other hand, for patients with conditions such as osteoarthritis of the knee, who cannot walk sufficiently but have no significant cardiac issues, we switch from metabolic mode to disuse mode with the aim of increasing muscle strength and muscle mass. Typically, after patients have undergone metabolic mode three times, we transition to disuse mode. From there, we gradually increase the intensity, targeting a maximum of mBorg 7 or above.

Post-B-SES implementation
Pre-B-SES implementation
Ochiai Kaori, Tamura Yuma, Yasu Takanori, et al.
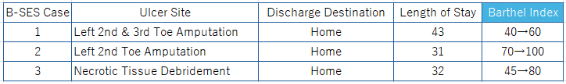
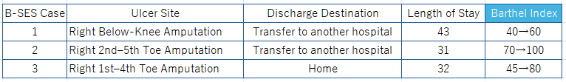
Bridge Therapy Using Belt Electrode Skeletal Muscle Electrical Stimulation (B-SES) in Patients with Peripheral Arterial Disease Presenting with Critical Limb Ischemia.
Physical Therapy Science, 2018.
Tamura, PT, PhD: Through the use of B-SES, I have observed that it synergistically enhances and accelerates muscle strength recovery in patients with significant muscle weakness when combined with conventional rehabilitation. Specifically, among patients with peripheral arterial disease (PAD), some present with critical limb ischemia (CLI). Before introducing B-SES at our hospital, three CLI cases took over two months to improve their Activities of Daily Living (ADL), as measured by the Barthel Index, and to be discharged or transferred. However, after implementing B-SES, similar improvements were achieved in approximately one month. I believe that this early recovery of muscle strength allowed for smoother progression to gait and transfer training, ultimately contributing to a shorter hospital stay.
Tamura, PT, PhD: At our facility, we currently have three B-SES units. Two are used for inpatients and outpatients undergoing cardiac rehabilitation, while the remaining unit is utilized in a dialysis unit with approximately 30 beds.In terms of usage, each cardiac rehabilitation device is typically used by about five patients. In the dialysis unit, an average of six patients receive B-SES treatment per day.
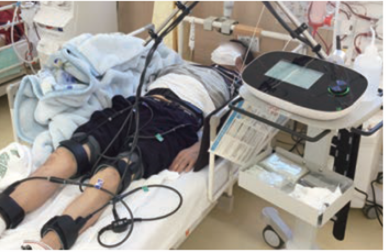
Photo: B-SES in Use at the Dialysis Unit
-Patient Feedback
Tamura, PT, PhD: The most common feedback we hear from patients is that their legs feel lighter. While our primary goal has been to increase muscle strength and enhance muscle metabolism, we believe that the muscle pump action induced by B-SES also provides a massage-like effect. Because of this, even in outpatient cardiac rehabilitation, having B-SES available seems to improve patient adherence — meaning patients are more likely to continue attending their sessions without dropping out. Additionally, we often hear reports of relief from musculoskeletal complaints such as lower back pain and leg numbness.
-Future Prospects for B-SES
Tamura, PT, PhD: Our goal for cardiac rehabilitation, as mentioned at the outset, is to use B-SES for cardiovascular disease prevention as well as for frailty and long-term care prevention. Currently, we are conducting a pilot study using B-SES with patients undergoing hypertension treatment, and the preliminary results are promising. If B-SES proves effective for hypertension, it could also contribute to preventing stroke, cardiac events, and potentially reduce the progression of care dependency.